The participants’ characteristics
In total, 2,027,353 subjects were included in this study. Among them, 308,354 (15.21%) had not received the COVID-19 vaccine (i.e., non-vaccinated subjects, no vaccination group in this study), whereas 1,718,999 (84.79%) were vaccinated against COVID-19 (i.e., vaccinated subjects, the vaccinated group in this study). The baseline characteristics of the vaccinated and non-vaccinated groups are presented in Table 1.
The cumulative incidences per 10,000 of psychiatric AEs following the COVID-19 vaccination
The cumulative incidence of the psychiatric AEs at three months was 0.51 (95% CI, 0.40–0.62) vs 1.98 (95% CI, 1.48–2.47) for schizophrenia, 18.30 (95% CI, 17.66-18.93) vs 14.24 (95% CI, 12.91–15.57) for depression, 0.79 (95% CI, 0.66–0.92) vs 1.39 (95% CI, 0.98–1.81) for bipolar disorder, 28.41 (95% CI, 27.62–29.21) vs 20.27 (95% CI, 18.68–21.86) for anxiety, dissociative, stress-related, and somatoform disorders, 0.30 (95% CI, 0.22–0.38) vs 0.32 (95% CI, 0.12–0.53) for eating disorder, 28.85 (95% CI, 28.05–29.96) vs 12.19 (95% CI, 10.96–13.43) for sleep disorders, 0.27 (95% CI, 0.19–0.34) vs 0.03 (95% CI, 0.00–0.10) for sexual disorders between the vaccinated group and non-vaccinated group. Therefore, the cumulative incidences of schizophrenia (p < 0.001) and bipolar disorder (p = 0.002) were significantly lower in the vaccinated group than in the non-vaccinated group. Meanwhile, depression (p < 0.001), anxiety, dissociative, stress-related, and somatoform disorders (p < 0.001), sleep disorders (p < 0.001), and sexual disorders (p = 0.007) showed significantly higher cumulative incidence in the vaccinated group than in the non-vaccinated group. There was no statistical difference in the cumulative incidence of eating disorders at three months between the two groups (p = 0.724). Detailed information of cumulative incidence was presented in Table 2.
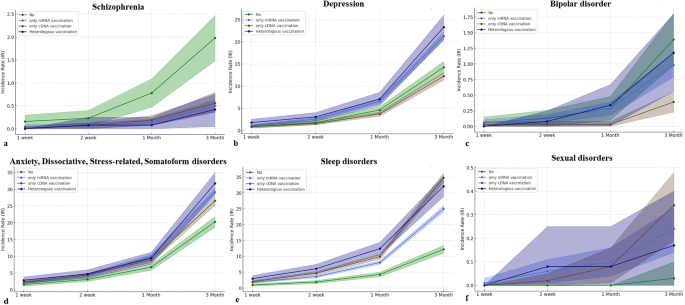
The cumulative incidences per 10,000 of psychiatric AEs according to vaccine types
Our data was also stratified by vaccine type including vaccination using mRNA-based vaccine only (only mRNA vaccine), vaccination using cDNA-based vaccine only (only cDNA vaccine), and heterologous vaccination, which were compared by non-vaccinated group. For decreased incidences of schizophrenia and bipolar disorder following COVID-19 vaccination, schizophrenia showed the lowest cumulative incidence at three months in the case of heterologous vaccination (0.42; 95% CI, 0.05–0.79) compared to other vaccine types with statistical significances (p < 0.001). The lowest cumulative incidence of bipolar disorder at three months was observed in the case of vaccination using only cDNA vaccine (0.39; 95% CI, 0.23-0.55) with a statistical difference (p < 0.001). For increased incidences of depression, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders following COVID-19 vaccination, the highest cumulative incidence of depression at three months was significantly observed in heterologous vaccination (23.31; 95% CI, 20.56–26.05) compared to other vaccine types (p < 0.001). However, the cumulative incidence of depression at three months was lower in the case of vaccination using only cDNA vaccine (12.26; 95% CI, 11.37–13.15) than in the non-vaccinated group (14.24; 95% CI, 12.91–15.57) with statistical differences (p = 0.014). The incidence of anxiety, dissociative, stress-related, and somatoform disorders was significantly observed to be highest in the case of heterologous vaccination (31.75; 95% CI, 28.55–34.95), followed by only mRNA vaccination (29.13; 95% CI, 28.08–30.18) and only cDNA vaccination (26.53; 95% CI, 25.22–27.83) (p < 0.001). The incidence of sleep disorders at three months was significantly observed to be high level in both cases of only cDNA vaccination (34.78; 95% CI, 33.28–36.28), and heterologous vaccination (32.09; 95% CI, 28.87–35.31), followed by only mRNA vaccination (24.98; 95% CI, 24.00–25.96) (p < 0.001). The cumulative incidences of sexual disorders showed no statistical differences up to one month (p > 0.05). At three months, the sexual disorder showed differences in cumulative incidence according to vaccine types (p = 0.04). There was no statistical difference in the cumulative incidence of eating disorders at three months (p = 0.785) according to vaccine types. The cumulative incidences of psychiatric AEs according to vaccine type are presented in Fig. 2 and Supplementary Table 2.
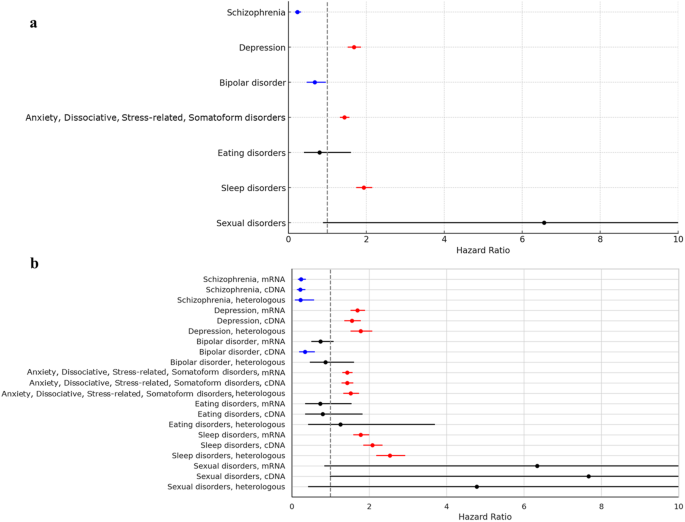
The risks of psychiatric AEs following the COVID-19 vaccination
In the Cox proportional hazard model in this study, the HR for COVID-19 vaccination was 0.231 (95% CI, 0.164–0.326) for schizophrenia, 1.683 (95% CI, 1.520–1.863) for depression, 0.672 (95% CI, 0.470–0.962) for bipolar disorder, 1.439 (95% CI, 1.322–1.568) for anxiety, dissociative, stress-related, and somatoform disorders, 0.796 (95% CI, 0.395–1.604) for eating disorders, 1.934 (95% CI, 1.738–2.152) for sleep disorders, and 6.556 (95% CI, 0.890–48.296) for sexual disorders. Therefore, COVID-19 vaccination significantly decreased the risks of occurrence for schizophrenia and bipolar disorder, while significantly increasing the risks for depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders. There was no effect of COVID-19 vaccination on the occurrence of eating disorders and sexual disorders (Fig. 3a).
In the multivariate logistic model in this study, the ORs of target psychiatric AEs, except for bipolar disorder at one week, two weeks, and one month showed statistical significance, indicating similar patterns for HRs in the Cox proportional hazard model. For bipolar disorder, the OR showed 1.166 (95% CI, 0.240–5.670; p = 0.849) at one week, 0.946 (95% CI, 0.304–2.949; p = 0.924) at two weeks, 0.982 (95% CI, 0.463–2.079; p = 0.962) at one month, and 0.674 (95% CI, 0.471–0.964; p = 0.031). The detailed information for ORs of target psychiatric AEs was described in Supplementary Table 3.
The risks of psychiatric AEs according to the COVID-19 vaccine type
We further assessed the risks of target psychiatric AEs according to the COVID-19 vaccine. For schizophrenia and bipolar disorder which were observed to have lower occurrences following COVID-19 vaccination, the HRs of schizophrenia were 0.239 (95% CI, 0.163–0.352) in only mRNA vaccination, 0.218 (95% CI, 0.138–0.343) in only cDNA vaccination, and 0.227 (95% CI, 0.091–0.566) in heterologous vaccination with statistical significances. On the other hand, the HR of bipolar disorder was statistically significant only in the case of only cDNA vaccination (0.339; 95% CI, 0.196–0.587). For depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders which were observed to have higher occurrences following COVID-19 vaccination, the HRs of depression (1.777; 95% CI, 1.527–2.067), anxiety, dissociative, stress-related, and somatoform disorders (1.521; 95% CI, 1.338–1.729), and sleep disorders (2.080; 95% CI, 1.855–2.332) showed the highest levels in the case of heterologous vaccination with statistical significances, respectively. There were no statistical differences in risks of eating disorders and sexual disorders according to vaccine types (Fig. 3b).
The ORs of target psychiatric AEs, except for bipolar disorder at one week, two weeks, and one month also showed statistical significance, indicating similar patterns for HRs in the Cox proportional hazard model. For bipolar disorder, the OR for only cDNA vaccination showed 1.581 (95% CI, 0.172–14.496; p = 0.685) at one week, 0.459 (95% CI, 0.073–2.893; p = 0.407) at two weeks, 0.191 (95% CI, 0.039–0.939; p = 0.042) at one month, and 0.340 (95% CI, 0.197–0.589; p < 0.001). The detailed information for ORs of target psychiatric AEs according to vaccine types was described in Supplementary Table 3.
Subgroup analysis for psychiatric AEs based on gender, age, insurance level, and CCI
As age increases, the risks of schizophrenia (HR, 1.027; 95% CI, 1.016–1.039) and sleep disorders (HR, 1.014; 95% CI, 1.012–1.016) significantly increase and the risks of depression (HR, 0.969; 95% CI, 0.966–0.971), bipolar disorder (HR, 0.982; 95% CI, 0.971–0.993), anxiety, dissociative, stress-related, somatoform disorders (HR, 0.988; 95% CI, 0.986–0.990) significantly decrease. Considering the HR values, age does not seem to largely affect the risk of psychiatric AEs. For the insurance level, the HR of schizophrenia at the high insurance level was 0.593 (p = 0.007) with statistical differences compared to the low insurance level. The HRs of depression at the high insurance level and middle insurance level were respectively 0.904 (p = 0.014) and 0.824 (p < 0.001) with statistical differences. There were no statistical differences in other psychiatric disorders for the insurance levels. For CCI, a higher score of CCI more than 2 significantly increased the risks of depression (HR, 1.393; 95% CI, 1.217–1.596), anxiety, dissociative, stress-related, somatoform disorders (HR, 1.440; 95% CI, 1.306–1.587), and sleep disorders (HR, 1.315; 95% CI, 1.198–1.444) than zero score of CCI. Based on these results, women are mostly susceptible to psychiatric AEs (except for sexual disorders) compared to men. Detailed information for Cox proportional hazard model for psychiatric AEs was presented in Supplementary Table 4.