
Many of us have come across research that tracks patterns of mental health problems throughout childhood and adolescence. Such research asks questions like: what proportion of the population experience mental health problems during childhood? What sub-groups can be identified? And how many individuals with a mental health problem worsen, improve or stay the same over the years?
Historically, longitudinal cohort studies such as the Dunedin study in New Zealand (Caspi et al., 2020) and ALSPAC in the UK (McElroy et al., 2017) have been the bread and butter of this type of research. In 2022, I was also involved in a study that used two longitudinal cohorts in Ireland to identify trajectories of symptoms throughout childhood (Healy et al., 2022).
However, a nagging question that plagues us all who use such datasets is: do longitudinal cohort studies capture “real life”? There is always the possibility that the individuals in these cohorts are a biased group—self-selected to be available and willing to participate, or “contaminated” somewhat by the repeated questioning throughout their lives.
The study being reviewed here has used real-life healthcare data to look at how young people interact with healthcare services for mental health support.

Do prospective studies really tell us much about the real-life use of healthcare? This study uses GP records to assess ‘real world’ use of healthcare services for mental health support in young people.
Methods
This study used the CPRD-Aurum system (which captures everyday information from 25% of GP practices across England), and two other data registers: Hospital Episode Statistics and Office for National Statistics. The sample included all patients aged 3-18 who presented to their GP with a mental health problem between 2000 and 2016. To be included in the study, the clinician must have included a code for a mental health symptom or diagnosis in the patient notes at that appointment.
The main aim was to group together individuals who showed similar patterns of (1) GP attendance, (2) prescriptions, and (3) contact with specialist mental health services, over the subsequent 5 years. These groups were chosen using group-based multi-trajectory modelling.
Results
369,340 individuals were identified as eligible from the primary care records. The authors found that 7 groups best captured different types of service-use in this sample in the 5 years after their initial presentation (see figure).
Just over half of the sample fell into group 1, who were characterised by low GP contact (after that initial presentation), low numbers of prescription medications, and little contact with specialist services.
The details of all other groups can be seen in Figure A. But I will draw attention to 3 key findings here:
- There were just 2 groups with persistently high prescriptions (groups 6 and 7) which made up ~15% of the sample. Over 60% of these individuals had been prescribed medication at their initial mental health presentation, rising to 80% in subsequent years. This group also showed relatively stable GP contact across the 5-year follow-up, with 40-50% of group 6 and 60-70% of group 7 seeing their GP each year.
- Some sex differences could be observed in groupings. For instance, females made up 60% of groups 3 and 5, which were characterised by high rates of depression and anxiety. Conversely, there was a slight majority (57%) of males in group 2, who were characterised by younger age at presentation, with issues such as autism, behavioural and conduct problems. However, these sex differences would not warrant labelling any group as a “male” or “female” group.
- For groups 3, 4 and 5, there were drastic changes in service use throughout the 5-year period. Group 3 saw a stepwise drop in all types of service-use each year after initial presentation. It is difficult to know whether this reflects improving mental health, or growing dissatisfaction with services. Groups 4 and 5 on the other hand saw sharp increases in GP contact and prescriptions several years after the initial presentation. Similarly, it is difficult to know whether these delayed escalations in service use reflect initial misdiagnosis, ineffective treatment, or simply a worsening of symptoms due to non-healthcare factors (e.g. adverse life experiences).
Finally, the authors investigated whether membership of any of these groups predicted time to (a) hospital admission for self-harm or (b) death by suicide. The majority group (low contact with services) was used as the reference group. Even after adjustment for potential confounds, most groups showed a significantly elevated risk of these two serious outcomes. The exception across both outcomes was group 3 who were characterised by the year-on-year drop in service use.
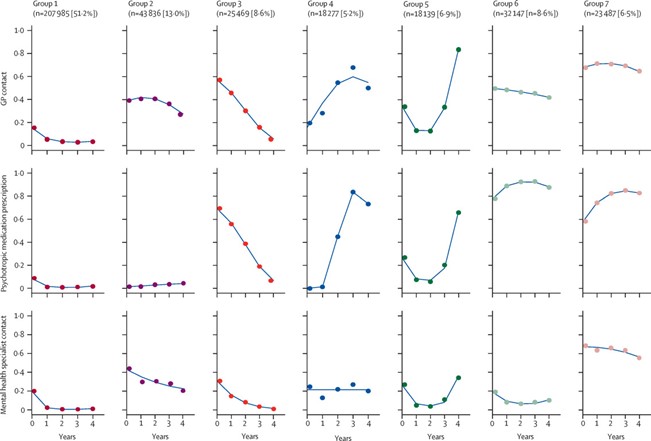
This study found that young people who contacted their GP for mental health support between the ages of 3 and 16 fell into one of seven groups, with over half of the sample being categorised by low engagement with GP, specialist services and prescriptions following initial presentation. [View full sized graphic]
Conclusions
The authors conclude that their findings may reassure children, adolescents & caregivers because 51.2% of children who presented to their GP with a mental health issue went on to have low contact with services. One might argue that this reassuring majority also includes group 3 (8.6%), who had decreasing service use over the 5-year period, and were not significantly different from the low-contact group in terms of subsequent risk of self-harm or suicide in adjusted models.
However, the authors emphasise that these results reflect service-use only. It remains difficult to say whether low contact with services reflects better mental health or disengagement with services due to unmet needs.

These findings may ‘reassure’ children, adolescents and caregivers given that 51.2% of children who presented to their GP with a mental health issue went on to have low contact with services.
Strengths and limitations
The major value of this study lies in its use of real-life primary care data, however this is also its main limitation.
One on hand, this study has strength in numbers due to its use of a national primary care database (CPRD-Aurum). It also has strength in ecological validity (avoids some selection biases) and clinical validity (all participants sought help for a mental health problem, arguably capturing non-trivial symptoms or functional impairment).
On the other hand, we could ask: who is really captured in this sample of children who have presented to their GP for a mental health issue? The answer is probably a complicated one involving the visibility of the child’s mental health issue, the child-carer relationship, stigma around mental health, trust in healthcare services and access.
Results from the Mental Health of Children & Young People in England survey (2021) showed that 1 in 4 parents do not seek professional help/advice for their child (aged 6-16) even when that child has a probable mental health disorder. The same survey also showed that less than half of older adolescents (and those in their early 20s) with mental health issues are likely to seek support in health services. Therefore, we could argue that this study sample may be biased toward those who have access to a GP service, feel comfortable presenting with a mental health issue, and toward mental health issues which are more visible or understood.
There are several other limitations of this study worth considering that the authors did not mention:
- Data-driven trajectories: In the statistics section of the paper, the authors explain how they tested alternative models with 1-7 groups to see which one showed the best fit to the data. The maximum number of groups (7) showed the best fit to the data which raises the question: while it might paint a more complex picture, is the number of groups that best capture the data greater than 7?
- Missed types of care: Specialist mental health care included “contact with psychiatrists, psychologists, or child and adolescent mental health services [CAMHS], or referrals for psychiatric symptoms or diagnoses”. But what is missing here? I wondered whether referrals from schools to CAMHS or disability services would be captured in the primary care system. Also missing from this list of specialist support are private counsellors including those accessed via web providers like BetterHelp, which have risen in popularity among adolescents (Ineqe Group, 2022)

The use of real-life primary care data is both a strength and limitation of this study.
Implications for practice
One of the key implications of this study is how routine GP data could be used to predict the care needs of a young person at initial presentation. There are both financial and health incentives to identify who will require intensive support ahead of time, and to curb service overload by delivering earlier or more appropriate intervention to those who need it. At a time when NHS mental health services are stretched, all efforts to make the system more efficient are worthwhile. However, my guess is that the authors did not mention this implication because there is quite a large piece of work to be done to extend these findings into accurate prediction modelling.
Another implication of this work for health service evaluators is the possibility of specialised mental health support to alleviate the pressure on primary care clinics. The results of this paper and others (Kontopantelis et al., 2021; NHS England, 2024) suggest that a small number of people may account for a disproportionate number of GP appointments. Take group 7 for instance: ~70% of these individuals attend their GP each year with a mental health related issue. Is the GP clinic the best form of support for these individuals? Could a specialised youth mental health service serve two purposes by (1) relieving pressure on GP services and (2) providing more specialised support to these young people? Such models of youth support are already in operation in Australia (e.g. Headspace) and Canada (e.g. Youth Wellness Hubs).
The authors note that more research needs to be done to supplement findings like these from health registers with more granular information on patient symptoms and functioning. I would add that qualitative input or patient and public engagement from young people (or their carers) who have sought help from their GPs for their mental health needs to be integrated with this type of data to truly understand how services work for this group.

Is the GP clinic the best form of support for young people experiencing recurrent mental health issues?
Statement of interests
No conflicts of interest to disclose.
Links
Primary paper
Senior M, Pierce M, Taxiarchi VP, et al. 5-year mental health outcomes for children and adolescents presenting with psychiatric symptoms to general practitioners in England: a retrospective cohort study. The Lancet Psychiatry. 2024;11(4):274-284.
Other references
Caspi, A., Houts, R. M., Ambler, A., Danese, A., Elliott, M. L., Hariri, A., Harrington, H., Hogan, S., Poulton, R., Ramrakha, S., Rasmussen, L. J. H., Reuben, A., Richmond-Rakerd, L., Sugden, K., Wertz, J., Williams, B. S. & Moffitt, T. E. (2020). Longitudinal Assessment of Mental Health Disorders and Comorbidities Across 4 Decades Among Participants in the Dunedin Birth Cohort Study. JAMA Netw Open 3, e203221.
Healy, C., Brannigan, R., Dooley, N., Staines, L., Keeley, H., Whelan, R., Clarke, M., Zammit, S., Kelleher, I. & Cannon, M. (2022). Person-Centered Trajectories of Psychopathology From Early Childhood to Late Adolescence. JAMA Netw Open 5, e229601.
Kontopantelis, E., Panagioti, M., Farragher, T., Munford, L. A., Parisi, R., Planner, C., Spooner, S., Tse, A., Ashcroft, D. M. & Esmail, A. (2021). Consultation patterns and frequent attenders in UK primary care from 2000 to 2019: a retrospective cohort analysis of consultation events across 845 general practices. BMJ Open 11, e054666.
McElroy, E., Shevlin, M. & Murphy, J. (2017). Internalizing and externalizing disorders in childhood and adolescence: A latent transition analysis using ALSPAC data. Comprehensive Psychiatry 75, 75-84.
NHS England (2024). News article: Two million more GP appointments for patients than before the pandemic. Published 15 Feb 2024.


